PayerWatch is the nation’s leading clinical revenue cycle and process improvement solution.
Is your hospital or health system equipped with the strongest tools and denial expert partners to effectively defend yourselves from payer denials and audits? PayerWatch is proven in over 500 hospitals nationwide.

Veracity
Revenue Protection Engine
Denials | Audits | Appeals
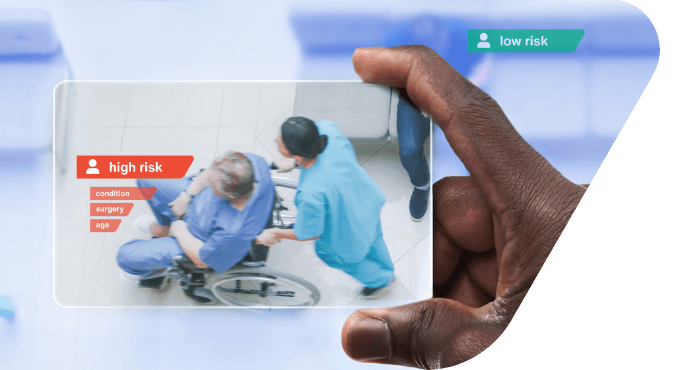
Dramatically increase your revenue protection and plug the payer leaks with our Veracity enterprise platform. Guaranteed.
- Denial prevention now
- Rapidly identify and fix broken processes
- Recover more revenue faster with fewer steps

- Clinical Validation Challenges
- Medical Necessity Denials
- Clinical/Legal Unit Approach
- Supporting 500+ Hospitals
PayerWatch Appeal Support Services
Supplement your internal resources with PayerWatch’s AppealMasters team of revenue recovery experts and complex payer appeal services. We’ll continuously train, educate and transfer knowledge as we help you win more appeals faster. Because performance improvement matters.
Advocacy, Training and Support
The Association of Healthcare Denial and Appeal Management (AHDAM) provides ongoing training and resources for all health care providers nationwide. AHDAM offers extensive training and education in denial and appeal management. Led by an expert team of denial and appeal management physicians, nurses, coders and attorneys.
PayerWatch is a fierce advocate for healthcare providers.
We empower you with the most efficient and effective tools to manage abusive payer practices, payer denials, payer audits and a winning appeal process.
Whether you’re leveraging the technological advancements of our Veracity revenue protection engine or supporting your internal teams with our expert AppealMasters support, PayerWatch is your trusted partner for revenue protection and defense. Over 500 hospital clients feel the same.
Preventing Denials to Increase Revenue
Veracity will not only help you get paid sooner and more often, but our solutions also drastically reduce the hard and soft costs associated with the administrative burden of audits and denials.
Enterprise Revenue Risk Management
Payer denials and audit takebacks are the unspoken black plague in Healthcare Revenue Cycle Management. Clinical denials, external audits, and the resulting lost revenue have been a blight on providers for too many years. PayerWatch’s Veracity platform presents a centralized platform for revenue risks across the enterprise – hospital, clinic, and ancillary denial and audit challenges that centralizes your responses, tracking, and healing your revenue at risk.
Finally – a flexible workflow engine for quickly fixing broken processes
Despite the attention and efforts that providers have dedicated towards denial prevention and audit management, improvements in re-capturing or retaining this crucial revenue remain difficult to achieve. PayerWatch’s Veracity platform identifies and fixes broken or inefficient revenue cycle processes quickly and effectively across all involved departments. Get it done today, not three months from today.
AppealMasters – Your lean and mean denial fighting machine
AppealMasters is the dedicated PayerWatch team of specialized clinical-legal appeal experts who serve providers by responding to all government and commercial payer denials and audits. Our professionals offer as-needed services and support from initial denial to ALJ hearings and External Review. Training, education, and process improvement recommendations are all included in our appeal support partnership.
Preventing Denials. Winning Appeals.
With AppealMasters, your organization benefits from winning appeal letters that include evidence-based medicine, NCD/LCD guidelines and state-specific legal arguments to support the appeal and reference specific findings in the medical record. Over 300 hospitals trust our expertise to appeal payer denials and audits through a comprehensive set of tools and services. Detailed reporting, corrective action recommendations, and collaborative insights are all part of being a dedicated team player with your staff.
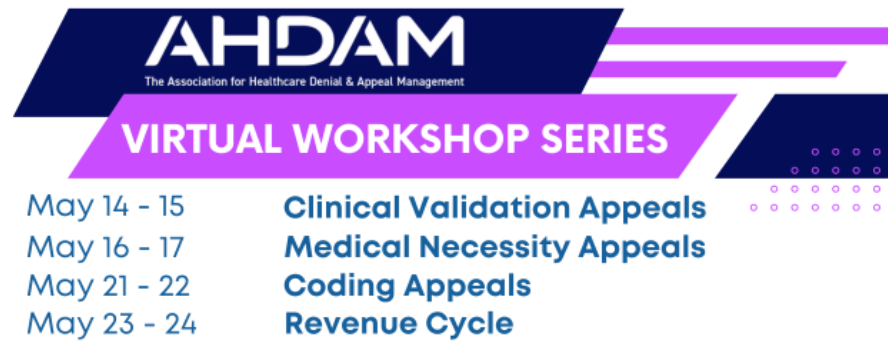
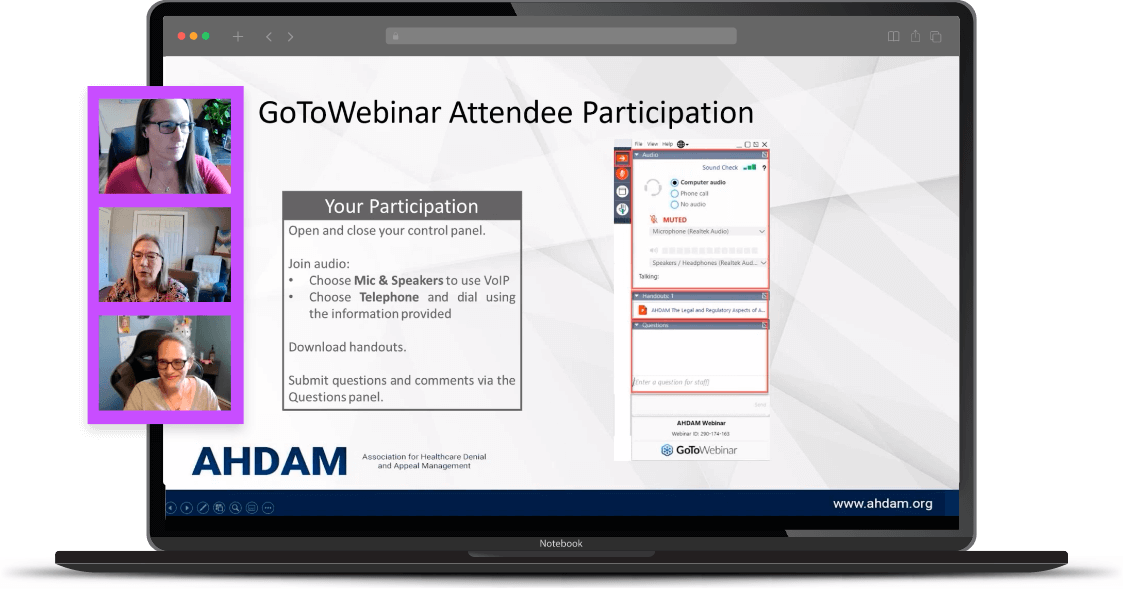
The Association for Healthcare Denial and Appeal Management (AHDAM) presents the 2024 Virtual Workshop Series. These interactive tracks are led by field experts who will dive deep into crucial topics that are vital to understanding the complex and ever-changing nature of the denial and appeal management process. This series is specifically designed for healthcare professionals who are involved in denial and appeal management and/or revenue cycle management.
Each two-day track runs from 11:00 a.m. – 3:00 p.m. ET with the opportunity to earn 6.0 CE credit hours and/or CMEs through AMEDCO, NAHRI, NEMSD, AHIMA, ACDIS, and/or PACE. See each course below for specific CE/CME offerings. You will have the option of registering for one or multiple tracks on the registration form.
PayerWatch AppealMasters Experts are Passionate About Making the Payers Pay
Our industry‐leading customer service is available to help and support everything you need to succeed in this incredibly challenging payer-provider environment. The PayerWatch staff are experts in medical necessity, clinical validation/CDI, coding, contracts, and legal protections who deeply understand the issues at hand and can help solve your denial, audit, and payer challenges. You get a serious, educated collaborative, and expert partner. Our Veracity and AppealMasters teams build close working relationships with your staff, who share in the service mission to improve processes and payment outcomes together.
Trusted Partners
PayerWatch has increased revenue for over 500 hospitals.
PayerWatch's industry-leading Veracity software and AppealMasters’ infrastructure is HITRUST CSF Certified.


